Dr. Jordan Sudberg on Navigating the Long Road to a Chronic Pain Diagnosis
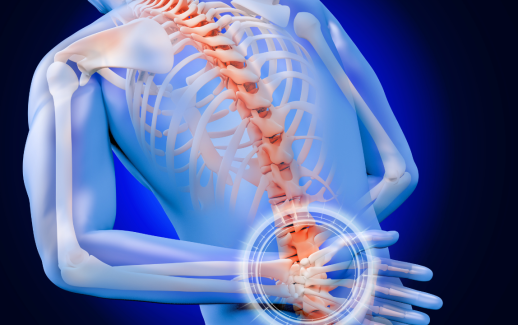
Living with chronic pain can be debilitating, but not having a diagnosis can make it even worse. For many patients, the search for answers can take months—or even years. Pain that doesn’t go away, that limits mobility and disrupts everyday life, often sends people from one specialist to another without clarity. Misdiagnoses, dismissive responses, and inconclusive tests only add to the emotional toll.
Dr. Jordan Sudberg, a leading pain management specialist, understands this journey intimately. Over his career, he has treated thousands of patients who arrived in his office not only in pain but also frustrated, discouraged, and desperate for answers. According to him, chronic pain is one of the most underdiagnosed and misunderstood medical issues in the healthcare system.
“Pain is subjective and complex,” says Dr. Sudberg. “It doesn’t always show up on scans or bloodwork, but that doesn’t mean it’s not real. Getting a diagnosis can be a winding road, but with the right approach, it’s absolutely possible.”
The Nature of Chronic Pain: Why It’s So Hard to Diagnose
Chronic pain is defined as pain that lasts longer than three to six months and extends beyond the normal healing period. Unlike acute pain, which is a clear signal of injury or illness, chronic pain often persists without an identifiable cause.
Common conditions that involve chronic pain include:
- Fibromyalgia
- Complex Regional Pain Syndrome (CRPS)
- Chronic fatigue syndrome
- Interstitial cystitis
- Migraines
- Myofascial pain syndrome
- Neuropathic pain
- Degenerative disc disease
But here’s the problem: these conditions often overlap in symptoms. A patient may experience widespread pain, fatigue, cognitive fog, and digestive issues—all of which can mimic or coexist with other disorders.
“Chronic pain doesn’t fit neatly into one category,” Dr. Jordan Sudberg explains. “That’s why so many patients feel like they’re being passed around the system. It requires a broad perspective and time to connect the dots.”
Step One: Listening to the Patient
The first step in diagnosing chronic pain is often the most overlooked: listening. Dr. Sudberg places a strong emphasis on comprehensive patient interviews.
“Patients are the experts on their own bodies,” he says. “We begin by asking about their full health history—not just their pain, but their sleep, stress levels, nutrition, activity, and emotional well-being.”
He also encourages patients to come prepared. Keeping a pain diary—including when symptoms occur, their severity, potential triggers, and related symptoms—can be incredibly helpful in spotting patterns.
Step Two: Rule Out Structural Causes
While many chronic pain conditions don’t show up clearly on imaging, it’s still critical to rule out structural issues such as herniated discs, arthritis, tumors, or fractures. MRI scans, CT scans, and X-rays help ensure that more serious conditions aren’t overlooked.
“Before we move toward diagnosing a functional or systemic disorder, we need to eliminate the obvious,” says Dr. Sudberg. “But that’s just the beginning—not the endpoint—of diagnosis.”
Step Three: Bloodwork and Laboratory Testing
Chronic inflammation, autoimmune markers, vitamin deficiencies, or thyroid dysfunction can also contribute to or mimic chronic pain disorders. A thorough blood panel may include:
- Complete blood count (CBC)
- Thyroid panel
- Vitamin D and B12 levels
- ANA (antinuclear antibody) test for autoimmune disorders
- ESR and CRP for inflammation
Dr. Sudberg notes, “You’d be surprised how many people suffer for years with undiagnosed autoimmune or metabolic issues that could be treated more effectively if identified early.”
Step Four: Multidisciplinary Evaluation
Because chronic pain is multifactorial, it often requires insight from multiple medical disciplines. Dr. Sudberg collaborates closely with neurologists, rheumatologists, psychologists, physical therapists, and even dietitians to build a 360-degree view of the patient’s condition.
“It’s never just about one body part,” he says. “Pain affects—and is affected by—every system in the body. Mental health, sleep, movement, nutrition—they all play a role.”
In many cases, co-existing conditions like depression, anxiety, or PTSD may intensify the perception of pain or make it harder for the body to heal. Dr. Sudberg stresses that addressing the mind-body connection is not only appropriate but essential.
Step Five: Functional and Diagnostic Injections
For certain musculoskeletal or nerve-related conditions, diagnostic injections can help confirm or rule out potential sources of pain. For example, a facet joint block or epidural steroid injection may indicate whether spinal inflammation is a key contributor.
“These tools aren’t just about short-term relief,” Dr. Sudberg clarifies. “They also help us pinpoint the exact location of dysfunction so we can treat it more precisely.”
The Emotional Toll of the Diagnostic Process
It’s not just the body that suffers during a lengthy diagnostic journey—the emotional strain can be overwhelming. Feelings of helplessness, invalidation, and isolation are common among chronic pain patients.
Dr. Sudberg is candid about the psychological burden his patients often carry: “The longer someone lives with unexplained pain, the more likely they are to experience depression, anxiety, or even trauma from medical gaslighting. It’s a vicious cycle.”
That’s why he advocates for compassion and validation throughout the diagnostic process. “Every patient deserves to be heard and believed. We don’t always get all the answers on day one, but we do commit to the journey together.”
Moving Forward with a Management Plan
Once a diagnosis (or at least a working diagnosis) is in place, the real work begins: managing the condition. Pain management is rarely about “curing” chronic disorders. Instead, the focus is on reducing symptoms, improving function, and restoring quality of life.
Treatment options may include:
- Physical therapy
- Medication management
- Cognitive Behavioral Therapy (CBT)
- Nerve blocks or injections
- Regenerative medicine (like stem cell therapy or PRP)
- Sleep and nutrition counseling
- Alternative therapies (acupuncture, mindfulness, etc.)
“Pain doesn’t define who you are,” says Dr. Jordan Sudberg. “With the right support and a customized plan, people can regain control over their lives—even if the pain never completely goes away.”
Final Thoughts: Stay the Course
Getting to the bottom of a chronic pain condition is rarely straightforward. It requires patience, perseverance, and partnership. If you’re still searching for answers, don’t give up. There are clinicians—like Dr. Jordan Sudberg—who are committed to walking the diagnostic journey with you, every step of the way.
“You may feel like you’re going to great pains just to be believed,” Dr. Sudberg acknowledges. “But don’t lose hope. A diagnosis is not just a label—it’s the first step toward healing.”